PMH recognizes National Volunteer Week | April 14-20, 2024
Written March 27, 2024
National Volunteer Week is celebrated this year from April 14-20, 2024. Volunteers undoubtedly make a difference in the health and well-being of the residents, patients, and clients that we serve within the Prairie Mountain Health (PMH) region. Over the last year, our healthcare volunteers have put in a collective total of over 37,000 hours!
“PMH sincerely values contributions made by our communities and stakeholders to our healthcare system,” says PMH Board of Directors Chair Lon Cullen. “Volunteers and volunteer organizations continue to play a significant role with our PMH team in supporting our Regional Vision of ‘Health and Wellness for All.’ We acknowledge and appreciate the heartfelt contributions that volunteers and volunteer organizations make directly or indirectly year-round!
The theme for National Volunteer Week 2024 is “Every Moment Matters.” It highlights the importance of every volunteer and each contribution they make at a time when we need support more than ever. Sharing time, skills, empathy, and creativity is vital to the inclusivity, strength, and well-being of our communities.
Volunteers support our personal care homes, hospitals, and community health programs across the region. Some examples include:
- Volunteers serve every personal care home within PMH, providing our residents companionship, entertainment and assistance.
- Dedicated volunteers who support the Palliative Care Program.
- A dedicated group of Pet Therapy Dogs/handlers (PATDogs Team) who take time from their day to bring smiles to the patients and residents in hospitals and Personal Care Homes. The PATDogs program was implemented in 2022 and has grown from three Therapy dog teams to 24 teams.
- Volunteers participate in local boards, foundations, auxiliary organizations, and other community meal and harm reduction programs.
- Volunteers assist with the Community Volunteer Income Tax Program.
These are just a few highlights of volunteer participation, dedication and commitment. It would be challenging to cover all the examples of how people selflessly give up their time.
“We very much appreciate our volunteers who dedicate their time, knowledge, compassion and heart to helping Prairie Mountain Health,” stated PMH CEO Brian Schoonbaert. “On behalf of our board, staff and physicians, we sincerely thank you for all you do from the bottom of our hearts. If you see a volunteer, thank them for making “Every Moment Matter.”
To apply to volunteer within PMH please visit our website Volunteer Services – Prairie Mountain Health.

Katherine Dwight is a dedicated volunteer for Boissevain Evergreen Place.
Katherine enjoys helping others, visiting with residents and assisting with recreation programs.
“To bring smiles to the residents is the biggest award” says Katherine.
Thankyou Katherine for your dedication to the residents and the PCH!

Eleanor is a dedicated volunteer at Rideau Park, Fairview PCH, and Minnedosa Care Home.
Eleanor began volunteering to help fill her need to do something musically.
“I love seeing a smile or hearing someone singing along.” says Eleanor.
Eleanor also enjoys singing, dancing and knitting.

Jessica is a dedicated volunteer at Rideau Park PCH.
Jessica began volunteering because she enjoys working with older people and was looking for somewhere to do that.
“Interacting with the residents is definitely my favourite thing about volunteering” says Jessica.
Jessica also enjoys cooking and baking.
Thank you Jessica for your dedication to the Residents at Rideau Park.

Alexe & Darlynne are dedicated volunteers at Dinsdale PCH & Fairview Home.
Alexe sings, and Darlynne plays piano. Together they provide wonderful music programs!
“My favourite thing about volunteering is the music & the residents – most love music. My friendship with Darlynne (pianist)…we’ve become very close.” ~Alexe~
“My favourite thing about volunteering is seeing the pleasure of residents & doing something I love!” ~Darlynne~
Alexe enjoys spending time with family, church and hobbies.
Darlynne enjoys spending time with family, church & other committees, computer skills, singing & playing, helping people who need assistance.
Thank you for sharing your love of music with residents around PMH.

Larry is a dedicated volunteer at Fairview Home.
Larry began volunteering when he saw a need for volunteers & his life changed, freeing up some time to give back to society.
“My favourite thing about volunteering is the joy & appreciation I receive from clients & staff. I always leave happier than when I arrived.”
Larry also enjoys volunteering his time with other organizations, fixing broken electrical & mechanical devices, and grandparenting.
Thank you Larry for sharing your time with Fairview Residents.
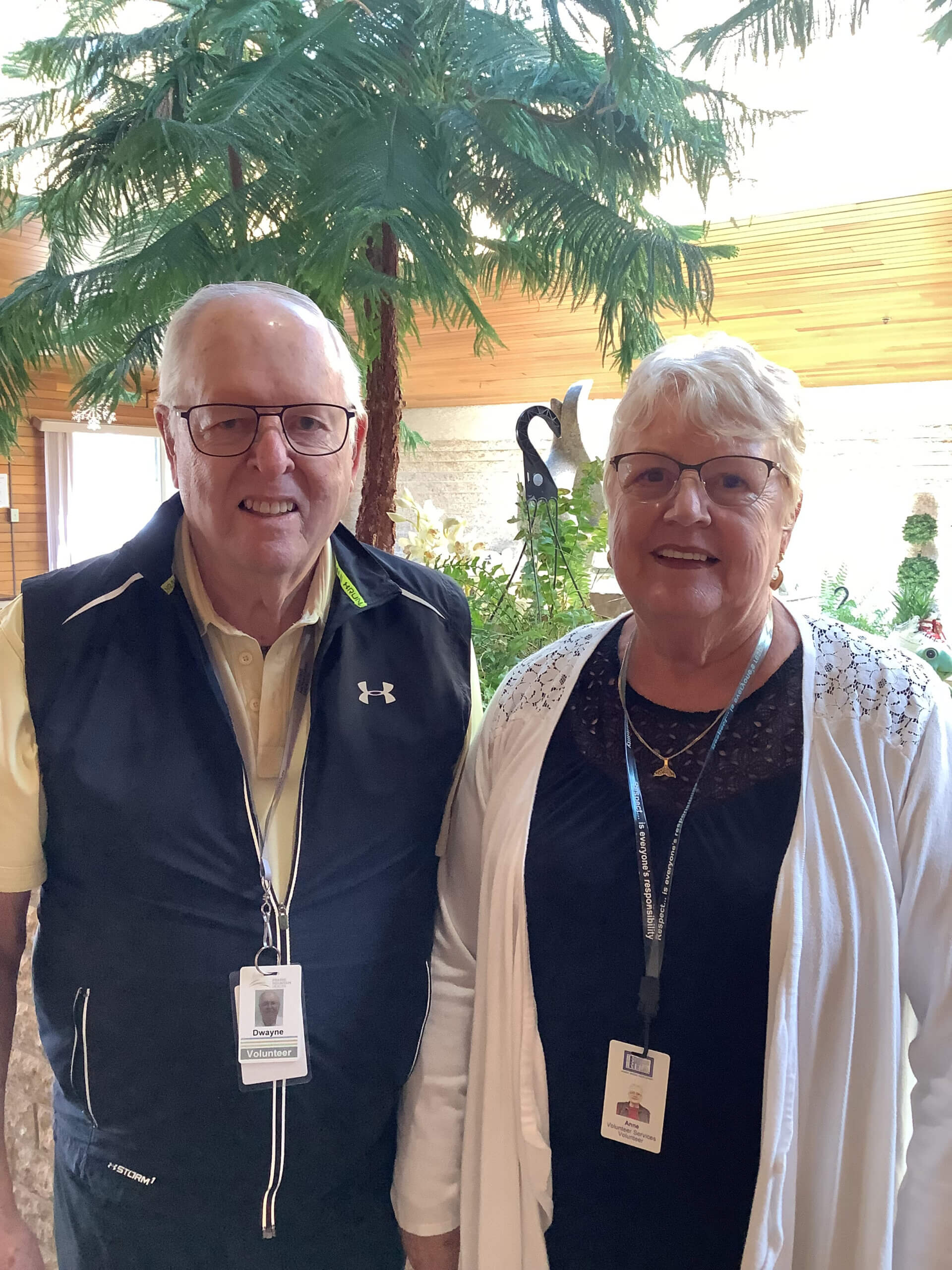
Dwayne & Anne are dedicated volunteers in Prairie Mountain Health.
Anne started volunteering when her mom was a resident at Fairview.
“My favourite thing about volunteering is working & talking with residents.”
Dwayne volunteers as a musician at Fairview, Rideau Park, & Dinsdale PCH
“My favourite thing about volunteering is playing music for the residents.”
Anne & Dwayne also enjoy curling, dancing, walking, travelling, and floor shuffling.
Thank you Dwayne & Anne for sharing your time with residents around PMH.

Melina is a dedicated volunteer at Fairview Home.
Melina began volunteering because she wanted to make a positive impact in her community. Volunteering offers opportunities to contribute her skills to meaningful places and connect with others.
“I love playing piano for the people and it’s nice knowing that some of them recognize me whenever I go now. It warms my heart every time I see them enjoy the music and the fact that my music can make them happy for that hour.”
Thank you Melina for sharing your love of music with the Residents of Fairview.
Carolyn is a dedicated volunteer at Dinsdale PCH.
Carolyn began volunteering when her mom was a resident at Dinsdale.
“My favourite thing about volunteering is socializing with the residents.”
Carolyn also enjoys jigsaw puzzles, cards and reading.

High Country Band has been sharing their love of music and friendship to residents for multiple years.
They perform monthly in the Personal Care homes in Sandy Lake, Erickson, Minnedosa and Neepawa.

Lorna McMillan is a dedicated volunteer at Delwynda Court in Deloraine with the recreation programs.
Thank you Lorna, for sharing your time with our residents.

Jan Russell is a dedicated volunteer at Rivers PCH.
Jan is a faithful recreation volunteer at Rivers PCH and loves her time volunteering and we love having her assistance and friendship!
Pictured left to right is one of our residents Louise, enjoying a game of crib with Jan.

Lenora Fassett is a dedicated volunteer at Rivers PCH.
Lenora is a faithful recreation volunteer at Rivers PCH and loves her time volunteering and we love having her assistance and friendship!
Pictured left to right is one of our residents Louise, enjoying her time with Lenora.